 Book Appt.
Book Appt.
 Call Now
Call Now


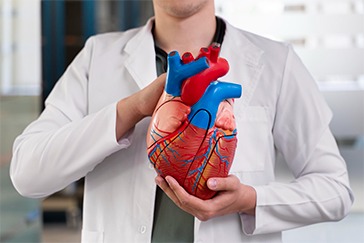
Pulmonary hypertension is a type of excessive blood pressure that affects the arteries in the lungs and on the right side of the heart. One type of pulmonary hypertension is pulmonary arterial hypertension (PAH), in which blood arteries in the lungs constrict, obstruct, or are damaged. The injury reduces blood flow in the lungs. Blood pressure in the lung arteries rises. The heart has to work harder to push blood through the lungs. The increased effort eventually leads the heart muscle to weaken and fail.
Symptoms
The symptoms of pulmonary hypertension emerge gradually. You might not see them for months or even years. Symptoms worsen as the condition advances. Symptoms of pulmonary hypertension include shortness of breath, blue or gray skin due to low oxygen levels, chest pressure or pain, dizziness or fainting episodes, quick pulse or pounding heartbeat, weariness, and swelling in the ankles, legs, and abdomen.
Causes
The typical heart has two upper and lower chambers. When blood goes through the heart, the lower right chamber pushes it into the lungs. The blood goes through the pulmonary artery, which is a main blood conduit. Blood typically flows freely from the lungs to the left side of the heart. These blood vessels comprise pulmonary arteries, capillaries, and veins. However, changes in the cells that line the lung arteries can cause the arterial walls to constrict, stiffen, expand, or thicken.
Pulmonary hypertension is classified into five types based on the cause.
Diagnosis
Pulmonary hypertension is hard to diagnose early because it's not often found during a routine physical exam. Even when pulmonary hypertension is more advanced, its symptoms are similar to those of other heart and lung conditions.
Tests
Treatment
Risk factors
Pulmonary hypertension is usually diagnosed in people ages 30 to 60. Growing older can increase the risk of developing Group 1 pulmonary hypertension, called pulmonary arterial hypertension (PAH). PAH from an unknown cause is more common in younger adults. Other things that can raise the risk of pulmonary hypertension are family history, being overweight, smoking, blood-clotting disorders, exposure to asbestos, congenital heart defects, living at a high altitude, and use of certain drugs, including cocaine or methamphetamine.
Prevention
It is not always possible to avoid pulmonary hypertension. Some risk factors are beyond your control. If you have risk factors, your doctor may suggest regular testing to monitor your heart and lung function. Taking steps to avoid or treat other medical issues can help reduce your chance of pulmonary hypertension. Create an exercise regimen, eat a heart-healthy diet, quit smoking and using tobacco, and take blood pressure and other prescription drugs as directed.
Conclusion
Pulmonary hypertension is a complicated and diverse illness that necessitates meticulous management and a proactive approach. While HIV presents substantial hurdles, continuous research and improvements in medical science offer hope for better treatments and results. If you or someone you know is having PH symptoms, seek medical attention right away. Early intervention can make a significant impact in maintaining heart and lung health, ultimately improving quality of life.
SHALBY Sanar International Hospitals provides extensive medical procedures backed up with our state-of-the-art technology and a team of highly qualified & experienced clinical experts.

Life-Changing TAVR Success Story | Dr. D.K. Jhamb | SHALBY Sanar International Hospitals

Timely Angiography Procedure Saves life of Iraqi Patient.

Rajiv Makhni, Managing Editor of NDTV, Shares His Experience at SHALBY Sanar International Hospitals

A successful treatment procedure helped Ms. Suri get over breathlessness
Our doctors pen down their research findings and experiences from time to time. Their words provide deep insight into the latest techniques, technologies and other advancements in healthcare. It provides expert answers to all kinds of health questions for real-life issues.
VIEW ALL



Since the day of its foundation, SHALBY Sanar International Hospitals is committed to provide comprehensive healthcare services. It regularly organizes awareness programs in its premises and encourages outdoor healthcare activities and camps with an intent to put focus on preventive healthcare.
VIEW ALL