 Book Appt.
Book Appt.
 Call Now
Call Now


Chronic pancreatitis is characterized by the long-term inflammation of the pancreas, a vital organ responsible for producing enzymes to aid in digestion and hormones like insulin to regulate blood sugar. This condition can result from various factors, including excessive alcohol consumption, gallstones, genetic factors, or certain medical conditions.
When is Surgery Considered for Chronic Pancreatitis?
Surgery for chronic pancreatitis is typically considered when conservative treatments, such as lifestyle modifications, medications, and dietary changes, fail to alleviate symptoms. The main goals of surgical intervention are to relieve pain, improve digestion, and manage complications.
Types of Surgical Procedures for Chronic Pancreatitis
Drainage Procedures:
Pancreatic Resection:
Considerations and Complications
Surgery for chronic pancreatitis is a significant undertaking and is not without risks and potential complications. Here are some important considerations:
Outlook
Surgery for chronic pancreatitis is a complex and carefully considered option when conservative treatments fail to provide relief. The choice of surgical procedure depends on the severity of the condition and the specific needs of the patient. Individuals with chronic pancreatitis must work closely with a healthcare team, including surgeons, gastroenterologists, dietitians, and pain management specialists, to determine the most appropriate treatment plan.
While surgery can improve the quality of life for many individuals with chronic pancreatitis, it comes with challenges, such as managing diabetes and adapting to dietary changes. Nevertheless, with the right medical guidance and support, many patients can achieve significant pain relief and better digestive function, allowing them to lead healthier and more comfortable lives.
SHALBY Sanar International Hospitals provides extensive medical procedures backed up with our state-of-the-art technology and a team of highly qualified & experienced clinical experts.

Patient from Iraq gets treated by Dr. Vinay Kumar Shaw | SHALBY Sanar International Hospitals

Patient from Vanuatu Treated by Dr. Vinay Shaw | SHALBY Sanar International Hospitals

Laparoscopic Cholecystectomy by Dr. Vinay Shaw | SHALBY Sanar International Hospitals

Amardeep Singh’s Journey to Recovery from Right Groin Hernia at Shalby Sanar Intenational Hospitals

Patient from Haryana undergoes Successful Soft Tissue Tumour Surgery | Shalby Sanar Hospitals

Mr. Omary Daudi from Tanzania Recovers from Morbid Obesity & Abdominal Wall Lipoma | SHALBY Sanar

Patient's Journey: Mr. Salih Mohammed from Iraq Recovers from Complex Fistula | SHALBY Sanar

Successful Laparoscopic Hiatal Hernia Treatment of patient from South Sudan by Dr. Vinay Kumar Shaw
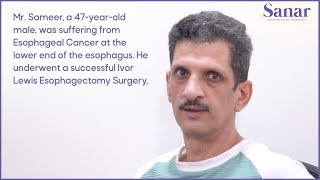
Mr. Sameer's Journey to Triumph: Overcoming Esophageal Cancer with Surgery

Empowering Transformation: Laparoscopic Sleeve Gastrectomy Success Story

Discover Minimally Invasive Laparoscopic Sleeve Gastrectomy Procedure

Success Story: Diya Ali's Gratitude After a Successful Minimally Invasive STARR Procedure -- Iraq
Our doctors pen down their research findings and experiences from time to time. Their words provide deep insight into the latest techniques, technologies and other advancements in healthcare. It provides expert answers to all kinds of health questions for real-life issues.
VIEW ALLSince the day of its foundation, SHALBY Sanar International Hospitals is committed to provide comprehensive healthcare services. It regularly organizes awareness programs in its premises and encourages outdoor healthcare activities and camps with an intent to put focus on preventive healthcare.
VIEW ALL